Introduction
Fertility is a journey that many women embark on with hope and expectation. However, when faced with ovulatory disorders, this journey can become complex and challenging. Ovulatory disorders are one of the leading causes of infertility in women, often shrouded in misconceptions and a lack of awareness.
This blog aims to demystify ovulatory disorders and their impact on fertility. Understanding these conditions is crucial for women who are trying to conceive and seeking guidance on this often difficult path. We’ll explore the different types of ovulatory disorders, their symptoms, diagnosis, and the various treatment options available.
Our goal is to provide a comprehensive, empathetic, and informative guide for women navigating the intricacies of fertility challenges. Whether you are just beginning to understand your fertility health or are already in the midst of managing an ovulatory disorder, this blog is here to offer support and knowledge. Through understanding, we empower ourselves to make informed decisions and keep hope alive in our fertility journeys.
Understanding Ovulatory Disorders
What are Ovulatory Disorders?
Ovulatory disorders are conditions where ovulation is irregular or absent, significantly impacting a woman’s ability to conceive. These disorders can stem from various causes, ranging from hormonal imbalances to lifestyle factors, and they affect a substantial number of women of reproductive age.
Types of Ovulatory Disorders
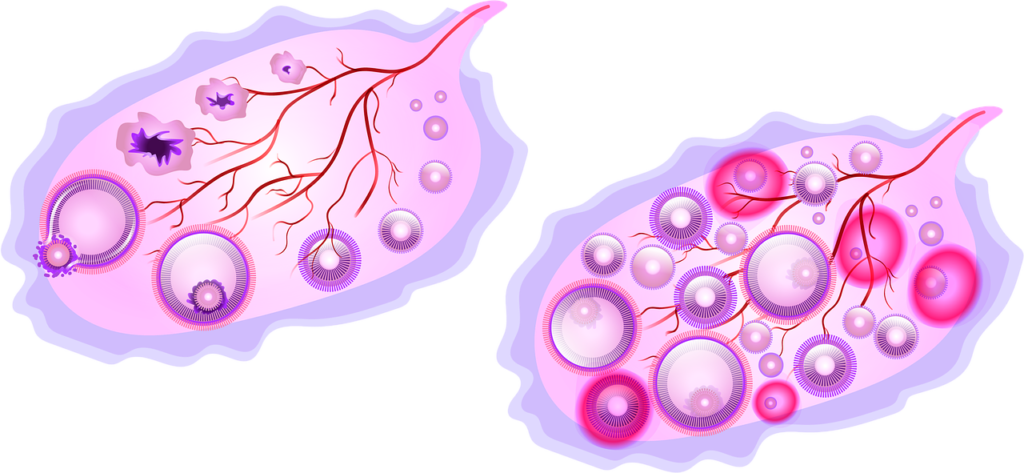
- Polycystic Ovary Syndrome (PCOS): This is a common endocrine system disorder among women of reproductive age, characterized by enlarged ovaries that contain numerous small cysts. PCOS often results in irregular or prolonged menstrual periods and excess androgen levels.
- Hypothalamic Dysfunction: The hypothalamus is an essential brain part that plays a crucial role in regulating the menstrual cycle. Factors like excessive physical or emotional stress, very high or low body weight, or substantial weight loss or gain can disrupt its function, leading to ovulatory issues.
- Premature Ovarian Insufficiency: This condition occurs when the ovaries stop functioning normally before age 40. It can result from genetic factors or certain autoimmune diseases.
- Excess Prolactin: The pituitary gland may cause excess prolactin production, which reduces estrogen production and may cause infertility. This condition can be due to medications or pituitary gland disorders.
Symptoms and Diagnosis
Symptoms of ovulatory disorders include irregular menstrual cycles, absent periods, excessive hair growth, acne, and weight gain. Diagnosis involves a comprehensive evaluation, including a medical history review, physical examination, blood tests to check hormone levels, and ultrasound imaging of the ovaries.
The Impact of Ovulatory Disorders on Fertility
The link between ovulatory disorders and infertility is significant. Ovulation is a critical process in the reproductive cycle, and any disruption can hinder a woman’s ability to conceive.
Understanding the Fertility Implications
Ovulatory disorders can lead to irregular or absent ovulation, which directly impacts fertility. For conception to occur, a healthy egg must be available for fertilization during each menstrual cycle.
Treatment and Fertility Outcomes
Fortunately, many ovulatory disorders are treatable. Treatments may include lifestyle changes, fertility medications, or even surgical interventions in some cases. The choice of treatment depends on the type of disorder and the individual’s overall health and fertility goals.
Treatment and Management Strategies
Managing and treating ovulatory disorders involves a combination of medical interventions, lifestyle modifications, and sometimes alternative therapies.
Medical Treatments
- Fertility Medications: Drugs like Clomiphene Citrate or Letrozole are often prescribed to stimulate ovulation in women with ovulatory disorders. In more complex cases, Gonadotropins might be recommended.
- Surgical Interventions: For conditions like PCOS, surgical options such as laparoscopic ovarian drilling (LOD) may be considered to induce ovulation.
Lifestyle and Dietary Changes
- Nutritional Adjustments: A balanced diet, particularly one that stabilizes insulin levels, can be beneficial, especially in PCOS.
- Physical Activity: Regular exercise helps maintain a healthy weight, which can significantly impact ovulatory function.
Alternative and Complementary Therapies
- Acupuncture and Herbal Medicine: These have been used to improve hormonal balance and overall reproductive health.
- Mindfulness and Stress Reduction: Techniques like yoga and meditation can help manage stress, which is beneficial for hormonal balance and overall well-being.
Coping with Emotional and Mental Health Aspects
Infertility can be a profoundly emotional and stressful experience. Managing these feelings is an essential part of the journey.
Addressing Psychological Impact
The stress, anxiety, and depression that can accompany fertility challenges are significant. Seeking professional help, like counseling or therapy, can provide crucial support.
Building a Support System
Connecting with others who are going through similar experiences, whether through support groups or online communities, can offer comfort and understanding.
Staying Hopeful
Despite the challenges, many women with ovulatory disorders successfully conceive. Advances in medical treatments and a better understanding of these conditions offer hope.
Conclusion
Ovulatory disorders present significant challenges in the journey toward parenthood, but they are not insurmountable. With the right information, treatment, and support, many women successfully overcome these hurdles. We encourage you to seek out professional advice, embrace healthy lifestyle changes, and lean on a supportive community as you navigate this path.
Remember, every journey is unique, and there’s always hope for a positive outcome.